Navigating the Complexities of NHS Income Management.
Insights from Helen Cookson.
As a former Associate Director of Finance with responsibility for Income and Contracting within NHS trusts, I have witnessed first-hand the intricate dance of balancing the books in the healthcare sector. I use the analogy of needing to land a jumbo jet on a 10p piece—a delicate operation that requires precision, foresight, and a bit of luck. Income is a key part of that process and often provides crosswinds, making landing on the 10p piece that bit harder.
The Challenge of Uncertainties
One of the most challenging aspects of income management is dealing with inherent uncertainties. As it can take up to five months for income to be crystallised, each month, we estimate our income based on incomplete and partially coded data.
These estimates are generated using a variety of methods, including historical trends, planned values, calendar days, and working days. However, inevitably there are variations in the estimate, which can be amplified by seasonal variations, lost commissioner challenges, and unexpected events.
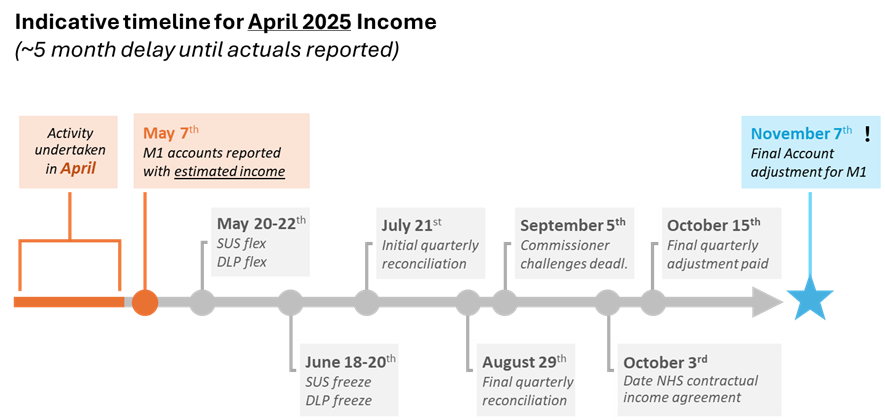
These estimates get baked into our financial reports and are often, particularly at the beginning of the year, rolled over into following months. Inevitably, these estimates lead to significant variations in our financial reports, which can be difficult to explain and manage.
The consequences of these variations can be severe. A sudden swing in income can throw an entire organisation off balance, leading to a loss of additional funding or even the imposition of special measures. This is why it is crucial to have a robust income management system in place. A good system allows for an earlier and more regular view of the income, rather than waiting until the month-end processes. Better tracking and more accurate reporting reduce the risk of errors and lost challenges, leading to a reduced risk of unexpected financial shocks.
Understanding the Bigger Picture
Effective income management is not just about the numbers on a spreadsheet; it is about the impact those numbers have on the organisation as a whole. A well-managed income system can provide the financial stability needed to invest in new services, improve patient care, and ultimately enhance the overall performance of the trust.
What Good Looks Like
So, what does good income management look like? It starts with accurate data and ends with informed decision-making. The three key themes that I have learned through experience, often the hard way, are:
1. Integrated Processes
Having an integrated income management process is crucial. This means ensuring that your income system is closely linked with your financial reporting and costing. Without this integration, you can end up with significant discrepancies that are hard to explain and manage. For example, if your income estimates are not aligned with your financial reports, you may face large swings in your reported income, which can undermine your credibility and financial stability.
2. Investing in Data Quality
High-quality data is the backbone of effective income management. Investing in data quality means ensuring that your income estimates are as accurate as possible. This involves regular data validation, cross-checking with other financial metrics, as well as using advanced analytics to identify and correct discrepancies and reduce commissioner challenges. Accurate data helps in making informed decisions and reduces the risk of unexpected financial shocks.
3. Clarity on Rules and Logic
Clear rules and logic are essential for consistent income management. This means having well-defined policies and procedures, supported by staff who understand and apply them with confidence.
In practice, though, many trusts rely on logic embedded in spreadsheets or legacy systems, making it difficult to trace or adjust. When estimation logic isn’t visible or easy to update, variations become harder to explain—especially as payment rules evolve. Bringing clarity means making your logic transparent, documented, and consistently applied. It helps ensure your reported position is both accurate and explainable—reducing risk and improving organisational confidence.
Why This Matters Now
Financial pressures across the NHS are intensifying. At the same time, the rules of the payment system continue to change, with evolving approaches. Expectations around data transparency are rising, and trusts are being held to higher standards of accuracy and agility.
In this context, improving income processes is not just a technical upgrade; it is a strategic necessity.
If you’re looking for ways to strengthen your trust’s financial position, improve credibility, and increase agility, income management is a smart place to start. You don’t need to do everything at once, but you do need to know what good looks like, and where you stand today.
I believe now is the time for finance leaders to lead the way—not just because the system demands it, but because it’s the surest path to stability and to delivering the care our communities deserve.
